Joe Murad, the new CEO of Vida Health, talks about his vision for the company
Murad was appointed last week, succeeding founding CEO Stephanie Tilenius
Read more...
While the idea of worksite wellness programs sounds great, giving employees incentives to get healthier and be more active, the sad truth is that they don't actually work very well; studies have shown that, while it's true that people do lose weight, they have not resulted in other numbers going down, nor in lower healthcare costs.
What does work, according to Blue Shield of California, is getting people to change their over lifestyle, rather than simply focusing on wellness, and the best way to do that is by giving people a choice in how they get to do it.
That's why the company announced earlier this week that it revamped its Wellvolution platform, first launched back in 2008, in order to help people improve their lifestyle in a way that fits their specific needs and preferences, making it more likely for it to have an overall effect on their health.
The program works like this: Blue Shield members are given survey questions to answer about things like their lifestyle and their health goals, as well how they would like to achieve goals. After that, they are matched with a personalized approach to their specific issue, which can include accessing mobile apps or online applications, as well as in-person resources and lifestyle-program resources, such as local gyms and community centers. Right now, there are more than 30,000 brick-and-mortar services on the platform, and nearly 70 digital health programs.
The new platform was created with digital healthcare marketplace Solera Health, which Blue Shield had previously worked with on a diabetes prevention platform.
Bryce Williams, vice president of Lifestyle Medicine at Blue Shield, spoke to VatorNews about the new program, the benefits of giving people choices in their lifestyle changes, and why he thinks traditional wellness programs are "zombies."
VatorNews: Talk to me about the new Wellvolution and how it works.
Bryce Williams: Let me start with the impetus of why we’re doing this. Our goal is pretty straightforward: improve the lives of those we serve. We recognize, as pretty much all the clinical evidence out there recognizes, that, in many cases, for most health risk factors or conditions, lifestyle is the most clinically effective, cost effective, least risky and least invasive option available. Not just for prevention but, even more importantly, the treatment and reversal of health risk factors in chronic conditions.
So, one of the distinguishing factors is us saying very, very clearly that isn’t about wellness, this isn’t about well-being; I mean, yes, it’s all there and it’s all good, there’s puppies and unicorns, but this is really about lifestyle medicine as a prescription-grade intervention, whether you want to prevent something, whether you want to treat something or whether you want to reverse something. And what we’re going to do to get you there is offer the largest community and digital therapeutic network of any health plan in the country, because, if we’re going to do that, we’re going to offer choice. We need to offer choice in what programs we’re offering because everybody’s different; they have different ways they want to go about doing diet and lifestyle, and they have different methods they want to go about doing it, whether it’s in person, whether it’s on the web, whether it’s on their phone.
And, finally, this is also about member preference and choice, not about your risk factor or, ‘You have a disease so you need to do this.’ It’s really about finding out what people want and then trying match them to be best option.
VN: How do you go about finding out what they want so you can match them?
BW: It’s this incredibly sneaky thing we do where we ask them. And that sounds really simple but, for some reason, healthcare tends to like to tell, not to ask. So, if you think about the way traditional health care and traditional health plans and traditional health management vendors go about it, it always starts with a history and a physical or a health risk assessment or some kind of lab screening or something like that. If you think about a health risk assessment, it’s largely this long and convoluted and arduous process where you have to answer a lot of questions about yourself that you already know the answer to, and then they tell you really interesting things that any semi-sentient second grader would know, like ‘Wear your seat belt when you get in the car,’ or ‘Don’t smoke, it’s bad for you.’ It’s just infantilizing and insulting.
Why don’t you just spend a couple of minutes with people when they come onto the platform? Instead of worrying about what risk they have, or what disease they have, or what’s their clinical condition, just say, ‘What do you want to do? Do you want to get more physically active? Do you want to stop smoking? Do you want to lose weight? Do you want to work on diabetes or high blood pressure? If you do, do want to to take meds? Do you want to try to get off meds?’ And then ask them questions about, ‘How do you want to do that? Do you want to do it in your neighborhood? In your backyard? At a local center? Would you rather do it online? Are you a group-based person? Do you like to be with people or do you like to fly solo? Do you like it in the palm of your hand? Do you like things via text? Via email?’ There are some basic questions you can just ask people.
Then what we do, because we have such a wealth of providers in the network, we can start to match you a little closer with what you want. We don’t have the hubris to think we’re going to get it exactly right the first time, but we offer members a first best match, and then right alongside it is a second best match. They can compare and flip and look between the two. If those don’t work they can go shop and look for something else.
The second aspect to this we don’t assume we’re going to get it right the first time. There’s a lot of times that all of us as human beings buy something and then we’re like, ‘I thought I wanted that but now that I try it, gosh darn it, I don’t think I do, actually.’ So, we offer frictionless switching so you’re not stuck in a program just because you got matched to it. You can choose something else, and that’s distinct from what you see from a lot of health plans as well. They’ll say, ‘Oh, you have type 2 diabetes, here’s the diabetes management program. You want to lose weight? Here’s the weight loss program.’ You ask, ‘What flavors do you have?’ and it's ‘Well, we have vanilla, vanilla and vanilla. Which one do you like?’ It’s really about just asking and then taking their feedback and adapting. I know it sounds crazy but, to us, it’s pretty simple human communication 101.

VN: You said in the press release that traditional wellness programs don’t work and you called them “zombies.” What do you mean by that? Why don’t they work?
BW: Let’s start with the facts: traditional worksite wellness, as a viable concept, died several years back. There’s been study after study after study after study saying that these traditional worksite wellness models don’t work. Yet, somehow, wellness vendors continue to offer them, employers continue to buy them, health plans continue to sell them, and so they’re like the zombie programs that just won’t die. You don’t need the evidence to be any clearer that they’re dead, but they shamble along and they cost employers and health plans a lot of money. Perhaps most tragically, they don’t do a whole lot to help the individuals that they’re supposed to be helping.
To answer the second part of the question about ‘why not?,’ it's because they’re not actually even designed to help, by and large. If you think about the core tenants of your average traditional wellness program, it’s around taking a health assessment, it’s around coming in every year to the conference room and getting a biometric screening or a blood draw, which, by the way, isn’t even clinically recommended consistent with clinical practice guidelines, so you’re already violating something that your doctor wouldn’t do. Some people might need to get their blood drawn every year, but not everybody. So, what you’re doing, at best, is you’re over screening and over testing and, at worst, you’re over diagnosing and sending people for additional tests and additional interventions that a) they probably don’t need and b) might actually be harmful. Then if you layer on, just to put the nail in the coffin, all of these financial incentives that go on top of this, from the relatively benign that don’t work and nobody cares about and just cost money, like gift cards, to the actually unhelpful, more coercive, cajoling, strong arming incentives like premium differentials tied to actual health outcomes, you end up in a very potentially dark place where you’re engaging with your members and employers from a place of force and coercion, versus a place of choice.
VN: What kind of ROI difference do you see when you give people a choice versus threatening them or coercing them?
BW: I guess this is going to sound radical coming from somebody from a health plan, but that’s not the primary motivation. One of mentors once said to me, ‘Do the right thing and the money will follow,’ and that’s truly what we’re after here. Most expenses in healthcare don’t generate a return, they’re costs, so what we’re most focused on is clinical impact. Before you worry about what kind of return are you going to get, you should worry about is it working? That’s what’s most important to us because these things are relatively inexpensive in the grand scheme of things. If you think that an once of prevention is worth a pound of cure, it’s true here: an ounce of investment is worth a pound of return, someday. But the first return I want to see is if we get the results that we expect. If we’re putting out physical activity applications, if we’re putting out weight loss applications, if we’re putting hypertension applications, or type 2 diabetes applications, what we want to see is: do people enroll? Do they stick with it? Do they get better, mentally, physically, spiritually? Do the numbers match up? So, do we see hemoglobin A1c coming down? Do we see weight coming down? Do we see blood pressures coming down? I don’t need to wait for any more studies to tell me that if people lose weight, get their blood sugar under control, get physically active, etc, that, eventually, they’re going to cost less. That’s not my primary motivation in doing this. Let’s do the harder work, which is find something that people like, that they’ll stick with and do.
Then I’d say the final success metric, which is perhaps even the most important, because it’s honestly the most real, is when people tell us directly, ‘This worked for me.’ That’s what improving the lives of those we serve really means. I know that sounds radical coming from a health plan, but financial ROI is not the primary motivator for doing this; in fact, it’s not even the secondary motivator, I’d say it’s a tertiary benefit if we get it.
VN: What kind of ROI have patients seen compared to other wellness programs? Have they lose weight? Have they been able to reduce their numbers?
BW: Wellvolution Next is literally two weeks old at this point, so I can’t tell you how it’s doing but I’ll tell you two statistics that are meaningful, the first of which is we are getting strong enrollment. We’re seeing a few thousand members enroll each week, which is a strong response, just being a couple of weeks in.
But perhaps what’s even most important and interesting to me is the distribution of the members that are coming in. We’re seeing about a 50/50 split between those members coming in who are looking to do, what I would call, general prevention activities. They want to get fit, they want to eat better, they want to stress less, etc. versus more intensive interventions like, ‘I want to avoid getting diabetes. I’m prediabetic, my doctors told me I’m at risk for diabetes, and they’ve given me a metformin prescription.’ Or, ‘I have high blood pressure and have one, two, three medications.’ Or, ‘I have type 2 diabetes and I have to take one, two, three medications.’ So, approximately half of our members are saying, ‘I want to work on the latter. I want to work on the harder things,’ and, perhaps even more importantly, ‘I want to use diet and lifestyle medicine to do it.’
So, one of the early differentiators is a lot of the stuff in the past has been just wellness for wellness' sake, and just assuming wellness is all about prevention, it’s not about treatment or reversal. Now we’re saying, ‘We’re going to give you an option. You choose. You want to do prevention, do prevention. You want to do diet and lifestyle more intensely? Or you want to do treatment or reversal?’ Half the people are saying, ‘Yes, I do.’ I haven’t asked them exactly why, but I’ve been doing this long enough that I have my suspicions: that it’s just a model that has never been offered to them. The traditional medical model has been a pill for every ill, or some kind of surgical intervention, and the only reason you do diet and lifestyle is fear of dying someday. And we’re flipping the script and saying, ‘No, it’s not about that at all, it’s about joy of living today.’ I could spend all day listing the benefits that come with it, but, honestly, you’re just going to feel better mentally, spiritually, physically and I think that’s what people are responding to early on.
Now, what I expect will happen is those numbers you talked about, because all of the partners, particularly the more clinical grade partners, that are in the network have been vetted because they come to the table with some level of scientific evidence, or randomized clinical trial publications, saying that what their interventions do, work. So, part of our vetting process is to say, ‘You don’t just get in because you’re a new digital health startup and you make promises, or you have a white paper, you have a lot of VC funding. I don’t care. What we want is some indication that you have done the hard work of actually doing some clinical trials to demonstrate efficacy.’ With our past experience with the diabetes prevention program, we’ve been able to work with our vendors, through our collaborative and competitive marketplace, to replicate the scientific studies, which is really hard to do. But we’ve been able to do it before and we have confidence we’ll be able to do it again.
VN: Can you give me some examples of some of those apps that are on the platform?
BW: We have 30,000 community partners, so those are brick and mortar locations, and we have around 40 partners and 70 distinct health and wellness applications in the market. That’s a lot when you think about your average health plan, which offers one or two or three.
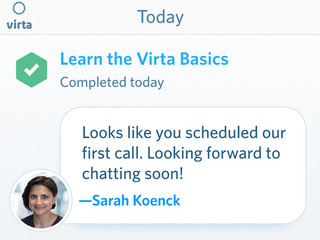
What we have is a nice mix of commercial applications you would readily recognize like WeightWatchers or PlateJoy and things of that nature, all the way up to some of the more digital therapeutics startups like Virta Health, WellStar and Better Therapeutics and BetterHelp and HealthSlate and Transform. You’re probably thinking that a lot of those vendors are in the same space, they’re actually competitors with one another, they’re chasing the same thing. That’s not by accident, that’s by design. Our thought is if we really want to accelerate and move the community and digital health field forward, we need to offer an accelerant marketplace where entrants can come in and collaborate and compete for market share and member mind share and, at the same time, demonstrate their results in a pay for performance environment.
VN: It makes sense to have multiple companies offering the same service, since that’s how you’re able to offer members choice in which one they want to pick.
BW: Absolutely and, for us, as a health plan, it’s hard picking a winner. This field is just growing so fast, there are new entrants every single day. We are not built to do that. That’s the old model, where you have one or two big entrants that kind of slog along again and again. When you have hundreds, thousands of new entrants, at any given time, the only way for us, as a health plan, to think about that is just to create an environment where if you demonstrate, get over the bar on scientific credibility and clinical protocols and safety, you’re in. Then we give you an opportunity to demonstrate; we’re going to help you succeed but, at the end of the day, it’s your fight, you gotta do it. So, from a health plan perspective, it’s beneficial too, beyond just member choice, but just for us not having to pick a winner in this space and, in essence, letting the membership and the clinical outcomes decide.
VN: Why was Solera Health a good partner? What do they bring to the table?
BW: Our initial relationship with Solera Health was around the diabetes prevention program and they helped us launch our community-based and therapeutic network. So, what they were really helpful in doing was giving us a platform where we could merge community-based providers, like YMCAs and fitness centers and JCCs and weight loss clinics, along with seven to 10 digital partners and put that in a marketplace where two things could happen: one, members could decide what they wanted to do when they wanted to address their prediabetes, and, two, we could manage and curate the network based on pay-for-performance metrics.
As that evolved over the last couple of years, and saw that a) members responded to it and b) that we were able to generate increasing positive clinical outcomes year-over-year, it really became kind of a virtuous success cycle as the partners learned from one another and tried to one up one another. They just all got better. We said, ‘Why would you just limit this to prediabetes?’ At that point you’ve built the technology, why not just scale the technology to other conditions, other health risks, other forms? Because the hard work’s already been done. So, they provide us that technology scaling component that we really need, as well as the ability to collect and manage the network and send us the claims billing for that as well.
VN: What is the ultimate goal with Wellvolution? What would success look like?
BW: I get up every day and come to work, and so does my team, to improve the lives of those we serve. To do that in lifestyle medicine, it’s pretty simple, this is dose-response medicine. To really have an impact, you need more engaged, doing it more frequently for a longer period of time. So, if I were to look ahead at success, in a year or two out we’d be seeing exponential growth, we would have come up with product and a message that resonates with people, and that people want to join, and they don’t want to join in a linear fashion, they want to join in exponential fashion. Also, I want to see the data back up that, if they want to get better, if they want to improve, that it’s quantifiable, it’s measurable, it’s demonstrable, and it’s meaningful. Finally, what would, for me, resonate the most is if just day after day after day after day I had members telling me their stories about their success and saying, ‘This is not what I expected from a health plan. I expected to get my claims paid and I expected to have a network of doctors available. I did not expect to have a lifestyle medicine program that would help me achieve my goals.’
VN: Is there anything else I should know?
BW: I would just reiterate, though you probably heard me say it five times, but it is kind of my north star, that we are here to improve the lives of those we serve. This is about lifestyle medicine, not general wellness. We’re doing it because everything has shown it’s the most clinically effective, cost effective, least invasive intervention. Not only prevention but also treatment and reversal, and the side effects are only positive. It’s not like a late night pharmaceutical commercial, where you see all these happy people and then it talks about dizziness, nausea, vomiting, incontinence and impotence and it’s like, ‘Wait, why do I want to take this?’ The benefits are only positive, like looking better, feeling better, loving better and that’s why we do this every day.
Murad was appointed last week, succeeding founding CEO Stephanie Tilenius
Read more...Noah Medical, which has developed a robotics system for detecting lung cancer, recently raised $150M
Read more...The company just announced a $22.5 million round, bringing its total funding to over $43 million
Read more...Startup/Business
Joined Vator on
The Virta treatment reverses type 2 diabetes and other chronic metabolic diseases, safely and sustainably, without the risks, costs, or side effects of medications or surgery. Our mission is to reverse type 2 diabetes in 100 million people by 2025.
Startup/Business
Joined Vator on
BetterHelp changes the way people get help to conquer life's challenges.
Facing obstacles alone can be daunting. Support and guidance from a professional counselor has been shown to make big changes. We created BetterHelp so anyone can have convenient, discreet, and affordable access to professional help.